A study conducted by Deloitte Access Economics in 2011 found that over 5 million Australians have incontinence (aged over 15 years) and 21% of individuals in community have incontinence in Australia1. A cross‐sectional survey conducted by another research group, reviewed 2,866 adults in 2005 receiving home care, and found that 17.6% had functional incontinence2
Functional Incontinence
Prevalence
Why does functional incontinence occur
This usually occurs due to either a cognitive or a physical issue that impedes an individual’s capacity to reach the toilet in time or to find the toilet, and can be exacerbated by environmental elements such as furniture in the way and clothes that are hard to get off.
Functional incontinence can affect individuals with a physical impairment related to a medical event or a disease, such as arthritis, stroke, multiple sclerosis, Parkinson's disease, motor neurone disease, and cerebral palsy to name a few. Diseases that can affect cognition such as dementia, stroke, brain tumours, an intellectual disability, and many neurological diseases in advanced stages, can lead to an impaired memory or ability to learn.
How does functional incontinence present?
This type of incontinence can present in the following ways
- An inability to undress and manage zippers, buttons, garments, pantyhose or continence aids to void or open bowels
- An inability to open the toilet door, turn the handle, lift the toilet lid, manage the toilet roll or taps due to such poor dexterity
- A lack of coordination or physical strength to perform the act of toileting or changing a continence aid due to a physical impairment
- An inability to find the toilet in the home due to memory issues
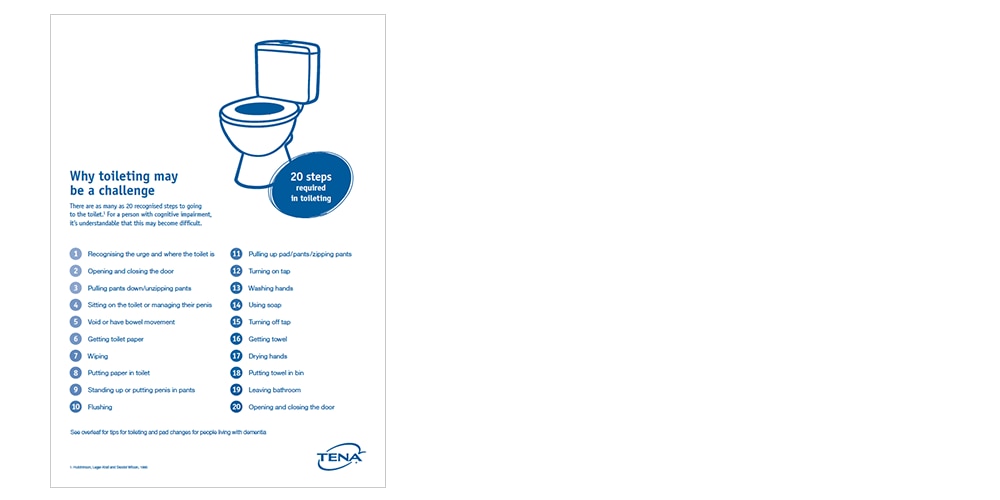
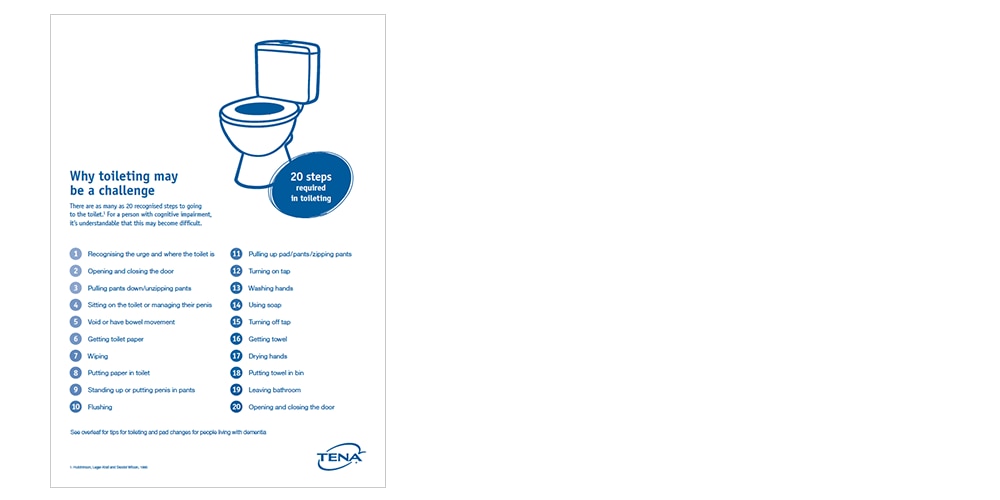
- An inability to recognise the toilet and remember the steps in toileting once in the toilet, due to an impaired memory. Toileting is a very complex activity and recent research has identified that it involves 20 steps. Information about this is included in our TENA Dementia Kit
- The inability to reach the toilet in time due to environmental obstacles such as furniture prohibiting entry or blocking the view to the toilet
How does functional incontinence present?
This type of incontinence can present in the following ways
- An inability to undress and manage zippers, buttons, garments, pantyhose or continence aids to void or open bowels
- An inability to open the toilet door, turn the handle, lift the toilet lid, manage the toilet roll or taps due to such poor dexterity
- A lack of coordination or physical strength to perform the act of toileting or changing a continence aid due to a physical impairment
- An inability to find the toilet in the home due to memory issues
- An inability to recognise the toilet and remember the steps in toileting once in the toilet, due to an impaired memory. Toileting is a very complex activity and recent research has identified that it involves 20 steps. Information about this is included in our TENA Dementia Kit
- The inability to reach the toilet in time due to environmental obstacles such as furniture prohibiting entry or blocking the view to the toilet
How can you assist a client managing functional incontinence at home?
1. Assist with physical issues
- Set up easier to use equipment in the toilet/bathroom - provide an “over toilet seat” with handles, arrange installation of grab rails to hold onto or better taps that are easy to use if needed or provide a wiping aid
- Provide education about appropriate clothing to make toileting easier- loose clothing such as track suit pants, elasticized skirts or pants, pants with a velcro fastening (no buttons or zippers) avoidance of pantyhose and safe footwear: non- slip sturdy slippers or stable shoes with a velcro closure
- Remove doors to the toilet if it could provide a safer access or advise the client to keep the door open at all times, if dexterity or strength are affected


1. Assist with physical issues
- Set up easier to use equipment in the toilet/bathroom - provide an “over toilet seat” with handles, arrange installation of grab rails to hold onto or better taps that are easy to use if needed or provide a wiping aid
- Provide education about appropriate clothing to make toileting easier- loose clothing such as track suit pants, elasticized skirts or pants, pants with a velcro fastening (no buttons or zippers) avoidance of pantyhose and safe footwear: non- slip sturdy slippers or stable shoes with a velcro closure
- Remove doors to the toilet if it could provide a safer access or advise the client to keep the door open at all times, if dexterity or strength are affected
2. Assist with memory problems
- Place a coloured sign on the door (with an image of the toilet) for easier identification (this is included in our dementia kit)
- Keep the door open at all times if it will assist
- Coloured taps, a coloured toilet seat, or coloured toilet paper (so they “stand out”)
- Images of taps above the taps, a simple diagram of steps in washing hands
- A hand towel for drying hands as opposed to paper towel (as it may seem more “familiar”)
- Also take notice of behavioural clues that may indicate someone needs to void or open bowels but cannot express it, such as restlessness, pulling at clothes, agitation


2. Assist with memory problems
- Place a coloured sign on the door (with an image of the toilet) for easier identification (this is included in our dementia kit)
- Keep the door open at all times if it will assist
- Coloured taps, a coloured toilet seat, or coloured toilet paper (so they “stand out”)
- Images of taps above the taps, a simple diagram of steps in washing hands
- A hand towel for drying hands as opposed to paper towel (as it may seem more “familiar”)
- Also take notice of behavioural clues that may indicate someone needs to void or open bowels but cannot express it, such as restlessness, pulling at clothes, agitation
3. Assist with environmental issues
- Ensure a safe a clear pathway to the toilet - remove furniture or rugs or other items that could be blocking safe access to the toilet
- Relocate furniture and rugs if necessary
- Remove mats from floor outside toilet door and in the bathroom
- Remove clutter in the bathroom or toilet
- Ensure there is good lighting
- Set up a commode or a urinal beside their bed for easy access to toileting (if toilet is difficult to enter or too far away for client)


3. Assist with environmental issues
- Ensure a safe a clear pathway to the toilet - remove furniture or rugs or other items that could be blocking safe access to the toilet
- Relocate furniture and rugs if necessary
- Remove mats from floor outside toilet door and in the bathroom
- Remove clutter in the bathroom or toilet
- Ensure there is good lighting
- Set up a commode or a urinal beside their bed for easy access to toileting (if toilet is difficult to enter or too far away for client)
4. Manage continence well
- Advise your client to wear a continence product, to give them confidence that they will not soil their clothing if they fear not reaching or finding the toilet in time
- For those with dexterity issues, usually a pull up pant product is easier to manage than a traditional pad in underwear (but it will also depend on client preference) So if a client has only one functional arm or hand, or has limited dexterity or weakness in their hands, this could be the best choice. See here for the link to our new TENA Quick Reference Guide to assist you in selecting the right product for your client.
- For those living with dementia pull up pants are the most like underwear, and cause less confusion
- Encouraging your clients to wear easy to remove clothing along with a continence product will also guarantee more success
- Understanding the normal toileting pattern of a client can help a client in setting up a routine at home, and hopefully avoiding accidents. We have a simple TENA Bladder Diary that a client or carer could easily complete at home, that could identify a bladder pattern and routine
- If you are unsure if it is not only functional incontinence and maybe a true incontinence, please arrange for your client to have a professional continence assessment by a qualified health care professional. Here is the link to our simple TENA Continence Assessment Tool


4. Manage continence well
- Advise your client to wear a continence product, to give them confidence that they will not soil their clothing if they fear not reaching or finding the toilet in time
- For those with dexterity issues, usually a pull up pant product is easier to manage than a traditional pad in underwear (but it will also depend on client preference) So if a client has only one functional arm or hand, or has limited dexterity or weakness in their hands, this could be the best choice. See here for the link to our new TENA Quick Reference Guide to assist you in selecting the right product for your client.
- For those living with dementia pull up pants are the most like underwear, and cause less confusion
- Encouraging your clients to wear easy to remove clothing along with a continence product will also guarantee more success
- Understanding the normal toileting pattern of a client can help a client in setting up a routine at home, and hopefully avoiding accidents. We have a simple TENA Bladder Diary that a client or carer could easily complete at home, that could identify a bladder pattern and routine
- If you are unsure if it is not only functional incontinence and maybe a true incontinence, please arrange for your client to have a professional continence assessment by a qualified health care professional. Here is the link to our simple TENA Continence Assessment Tool
*Required fields
*Required fields
*Required fields

TENA assist – sampling and education
Health care professionals can access samples for their clients, so they can try products before making a decision on a product to use. Here is a link to sign up to our TENA assist program that also gives access to various educational material for Health Care Professionals. TENA assist membership give you access to our nurse to discuss products, service or challenging situations.
Need help with continence product advice?
Call our friendly customer service team on
Australia 1800 623 347
New Zealand 0800 443 068
Where to buy TENA products
TENA products are available at Supermarkets and Pharmacies as well as homecare delivery distributors such as:
www.brightsky.com.au
www.independenceaustralia.com.au
direct.ch2.net.au
References
- Deloitte Access Economics Pty Ltd. The economic impact of incontinence in Australia. Melbourne; 2011
- Prevalence of urinary incontinence among community‐dwelling adults receiving home care M.F.M.T. Du Moulin, J.P.H. Hamers, A.W. Ambergen, M.A.P. Janssen, R.J.G. Halfens 06 June 2008; https://doi.org/10.1002/nur.20291



